Services and case studies in Quito
Services in Quito
Brain surgery
Procedures to treat problems in the brain and surrounding structures
Brain tumors
Brain tumors comprise a large group of varied lesions that manifest in different ways. Treatment goals and recommendations are therefore very diverse and tumor-specific.
First, a diagnosis is sought. Sometimes magnetic resonance imaging (MRI) is sufficient to give a confident diagnosis, but it is usually necessary to take tissue samples at the time of surgery. This may be done through a biopsy or by performing a resection of the tumor. Recently there has been some significant progress in the genetic analysis of tumor samples, in addition to the standard “microscopic” appearance to help make treatment decisions. This is particularly true for “gliomas” and other “primary” tumors.
The two broad categories of brain tumors are primary tumors (arising from brain tissue) and secondary tumors (starting outside the brain and traveling or compressing the brain). Some brain tumors are biologically benign. These tumors do not need postoperative treatments unless there is recurrence or a potentially aggressive pathology. Many primary tumors and the vast majority of secondary tumors will require additional postoperative treatment: either radiation therapy, chemotherapy or both.
The benefits of an initial tumor resection include: diagnostic accuracy, relief of direct and indirect pressure effects, potential cure and, in many cases, improvement in overall outcome by assisting adjuvant postoperative treatments. Surgical planning and recommendations are of course highly individualized and depend on a variety of factors. Clinical and radiologic evaluation will help determine the risk and benefits and, therefore, the appropriateness of surgery.
Glioma
This is a very broad term that describes a group of tumors originating from “glial” or supporting cells of the brain. These tumors range from low grade and slow growing to high grade and fast growing. The treatment depends on the type and grade of the tumor, as well as on a number of clinical factors. Tissue sampling or biopsy is necessary to establish the diagnosis. Various subtypes include astrocytoma, GBM (glioblastoma multiforme), oligodendroglioma, ependymoma, medulloblastoma, neurocytoma and ganglioglioma.
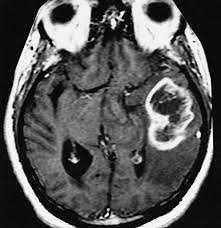
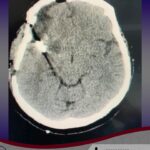
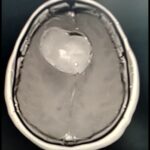
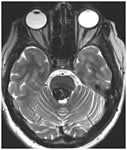
A Glioma that causes compression effects and “edema” (swelling).
GBM (Glioblastoma Multiforme)
This is the most common type of a primary brain tumor and nearly always requires surgery. Given that the tumor is intrinsic and that it grows around nerve fibers, it is usually not possible to cure it. Instead, most of the accessible tumor will be safely removed. After the operation, radiation therapy and chemotherapy are administered. Genetic testing of the tumor is also very helpful in determining the best treatment.
Low-grade gliomas
A low-grade glioma is usually a slow-growing lesion with a characteristic appearance on MRI and CT scans. Treatment remains controversial and varies from observation only to biopsy or resection (removing the tumor).
Meningioma
These tumors start outside the brain and usually compress it slowly. They have a very characteristic appearance on MRI and CT scans. Surgery is recommended when there is tumor growth on serial imaging, tumor-related symptoms or uncertainty with the diagnosis. Surgery is usually quite simple in this case, depending on accessibility, and patients are often effectively cured. However, long-term MRI surveillance is recommended.
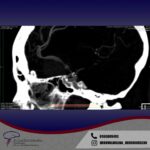
Acoustic neuroma (Schwannoma)
This special type of tumor has a higher degree of complexity and may occur as part of an inherited syndrome. The tumor arises from the balance and hearing nerve and therefore patients often experience hearing loss. This tumor is also closely related to nearby cranial nerves and can cause compression and dysfunction of the underlying brainstem. Treatment decisions depend on a myriad of factors, but range from periodic observation and monitoring, surgical resection or volume reduction, or treatment with stereotactic radiation (radiosurgery).
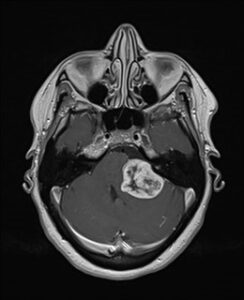
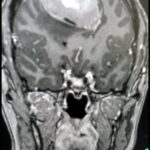
A large acoustic neuroma with brainstem compression.
Metastatic cancer
When a primary tumor spreads from its place of origin, it is usually transported by the bloodstream. The brain is an important site for secondary deposits and these tumors have a very characteristic appearance on MRI. They often cause substantial brain swelling. If the primary site is unknown or if one or more lesions are symptomatic and accessible, surgical removal is usually recommended.
Pituitary tumors
Pituitary tumors are a specific group of lesions that are located below the visual apparatus (optic nerves) at the base of the skull. When there is sufficient enlargement, these tumors can cause visual disturbances by compressing the optic nerves or chiasm from below. They also often present hormonal imbalances called endocrinopathy, either because of too much or too little of a specific hormone. Due to their location in the midline immediately behind the nose, they are easily accessible with minimally invasive approaches in case of a surgical intervention. In other words, they can be surgically removed through the nostrils.
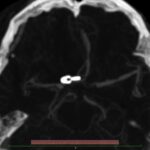
Hydrocephalus
Hydrocephalus refers to a problem with the normal circulation of “CSF” (cerebrospinal fluid) through the deep chambers or ventricles of the brain and around the special fluid spaces around the brain. It leads to a buildup of intracranial fluid and/or pressure, which can cause a number of neurological problems, such as headaches, trouble walking and difficulty with cognitive performance (thinking and memory). In its acute forms it can be imminently life-threatening. Occasionally, the cause is a blockage within the fluid chambers, blocking from the inside, but more often, no discrete blockage is seen and the problem is to be found in the spaces surrounding the brain or in fluid absorption. The most common way to treat this problem is with a “ventriculoperitoneal shunt”, but in some cases a “third ventriculostomy” (minimally invasive endoscopic procedure) will effectively prevent acute hydrocephalus.

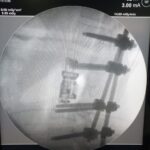
Ventriculoperitoneal shunt placed for “hydrocephalus”.
Chiari Malformation
Chiari malformations comprise a group of developmental disorders that result in an abnormal position of the “hindbrain”. The most common type is a type 1 lesion, where part of the balance structure called the cerebellum is positioned too low. This leads to compression of the underlying brainstem and secondary problems with fluid accumulation. When symptomatic or when there are obvious pressure problems, surgical intervention is recommended. The goal of surgery is to create enough space at the site of the obstruction to relieve compression and prevent further fluid pressure buildup.
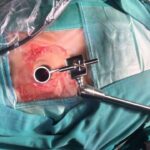
Trauma
Trauma can result in a wide range of neurosurgical problems. Occasionally, the trauma is so trivial that there is no memory of the actual event. The most common problem needing treatment is a “subdural hematoma” and “epidural hematoma”. Surgery is recommended if there are pressure effects on the brain or symptoms of compression. The recommended intervention ranges from a simple trepanation hole (trephination) to removal of the clot through a major craniotomy/craniectomy (removal of a part of the skull).
Aneurysms
Aneurysms are bulges in an arterial wall that represent weak points. They are found in about 2-3% of the population and usually remain undetected until they rupture. A ruptured aneurysm leads to a very severe headache and a rapid onset of neurological problems. The characteristic pattern of hemorrhage is called a “subarachnoid hemorrhage.”
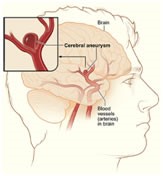
Aneurysms can also cause instant death or result in permanent disability. In some cases, there is a strong family history or genetic condition. The most common inherited disorder is adult polycystic kidney disease. Trigger factors for aneurysm rupture include smoking, poorly controlled hypertension, and overexertion. If left untreated, there is a cumulative annual risk of rupture and periodic screening is recommended.
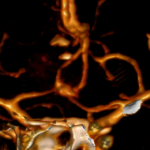
The typical bleeding pattern is seen after aneurysm rupture. The shape and location of the aneurysm can predict its behavior and also determine which treatment is preferred. Alternatively, if the aneurysm has a low risk of rupture or a high surgical risk, we may choose to surveil it with serial imaging. The intervention is designed to block the blood flow into the aneurysm, therefore eliminating the risk of hemorrhage. It can be performed endovascularly – by filling the aneurysm from within (“endovascular coiling”), or by open microsurgical techniques (“clipping”).

Surgical clipping (resolution)
A small incision is made behind the hairline and a piece of bone is removed to allow access to the aneurysm. The aneurysm is identified under microsurgical vision, with its branches and one or more clips applied externally to its neck. When the aneurysm is healed, the bone is replaced with special titanium plates and the incision is closed.
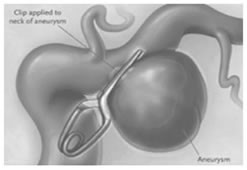
Clipped aneurysm

Aneurysm clip and support
- Arteriovenous malformations (AVMs)
Arteriovenous malformations or AVMs are congenital anomalies that affect the blood vessels in a specific region of the brain. They result from a disruption of the normal, progressive sequence of blood vessel wall type from artery to capillary to vein. Instead of this sequential change, there is a nidus or tangle of vessels under arterial pressure, which diverts blood directly from the high-pressure arterial circulation to the venous circulation, with no slowing down and little decrease in pressure. The result is constant high flows and elevated pressure throughout the AVM. This generates abnormal vessel shear stress and can lead to vessel wall rupture and spontaneous hemorrhage.
In addition to the local consequences of high flow and elevated venous pressures, the nearby brain is deprived of its blood flow. This is particularly true with large AVMs and can result in what is known as the “steal” syndrome. This can cause neurological problems, if the nearby brain is functionally important or “eloquent”. AVMs can manifest in spontaneous hemorrhage, seizures, a neurological problem or deficit, or headaches. With CT and MRI being much more prevalent these days, they can also be found incidentally.
Treatment decisions are based on balancing the estimated risk of immediate and future bleeding (“cumulative lifetime risk”) versus the risk of eradicating the lesion with treatment. Clearly, despite the use of complex tables and statistical methods, it is not possible to know with certainty the natural history of any individual. It is stated that the annual risk of hemorrhage associated with an AVM lies between 2 and 4%. There are certain risk factors that may increase this likelihood, such as a previous hemorrhage, arterial or intranidal aneurysms, restricted venous flow, and underlying respiratory or medical conditions. Each hemorrhage also entails the possibility of death or stroke and disability.
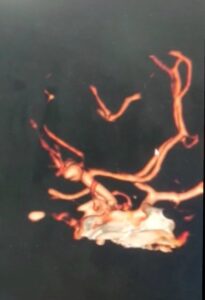
Several imaging modalities can be used to define the AVM. Computed Tomography (CT) and its variant Angiotomography provide information on the location and static vascular anatomy, including the vessels supplying and draining the AVM. Magnetic resonance not only tells us where in the brain the AVM is located, it also helps to measure risk and surgical approaches and provides information on previous hemorrhages. Cerebral angiography provides detailed dynamic information on flow patterns and venous drainage. Although it is the most sensitive and powerful test, it is also technically more “invasive” and entails a very small risk of stroke.
Treatment recommendations can range from observation and medication to microsurgical excision, but other forms of treatment are becoming more prominent worldwide. The internal blocking of the arterial feeders, through the artery, is called “embolization” and is extremely helpful in making the surgery safer. It is usually a preoperative maneuver. Occasionally, it may be the only treatment required.
Malformation
Post-resection
Arteriovenous malformations can also be cured with “radiosurgery”. This procedure involves the use of powerful computers to direct an array of radiation beams into the AVM volume. AVM shapes are often complex and a great deal of planning is needed in targeting them. This form of treatment does not have an immediate effect and results in slow obliteration of flow within the AVM over several years. Of the low-volume lesions that are treated, 70 to 85% will heal. MRI and progress angiograms are needed to establish a cure. Lesions of 3 cm used to be the upper limit in size for targeted lesions, but it is possible to treat larger lesions if the “marginal” dose – the dose that is directed towards the edge of the lesion – is reduced. A correct marginal dose is needed to obtain the best balance between lesion healing and brain protection.
Radiosurgery planning

Linac Stereotactic Radiosurgery
Cavernous malformations
Cavernous malformations are focal collections of thin-walled widened vessels under low pressure and low flow. There is usually evidence of previous hemorrhage in or around the lesion and they have a very characteristic magnetic resonance (MR) appearance. Familial forms occur and may be solitary or multiple. They may manifest in seizures, neurologic events or hemorrhage or may be discovered incidentally. The lesions that do not cause symptoms are observed with MRI. Accessible symptomatic malformations are eliminated.
A cavernous malformation of the brainstem.
Moyamoya disease
Little is known about Moyamoya; a disease of the main arteries at the base of the brain. In response to the progressive narrowing seen in the large arteries, a network of thin vessels forms in an attempt to maintain blood supply to the starved brain. The condition shows Transient Ischemic Attacks (TIA) or ischemia, or intracerebral hemorrhage. Cerebral angiography can provide a definitive diagnosis. Treatment consists of a variety of strategies from observation to extracranial-intracranial bypass surgery. Endovascular treatments are not usually recommended because of vessel fragility and restenosis. In addition, some relatively simple procedures can improve blood flow and help with symptoms.
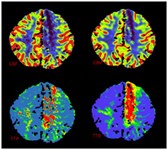
Typical CT perfusion findings in someone with Moya Moya’s disease

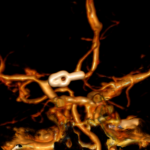
Recurrent aneurysm seen near clips
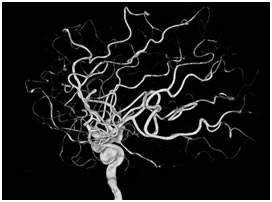
3D brain angiography showing an aneurysm
Services in Quito
Spine surgery
Correction of possible structural anomalies
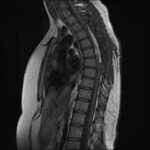
Disc disease
Disc disease is probably the disease most frequently treated by neurosurgeons and spine surgeons. Acute disc prolapse, bulging disc, herniated disc or ruptured disc are terms commonly used to describe failure of this structure. When symptoms are new, the typical sequence is first back pain in the region of the disc followed by nerve irritation pain in the arm or leg. This is called radicular pain, and some people use the term sciatica when the leg is affected.
A long-standing prolapsed disc may lead to chronic back, neck, arm, shoulder or leg pain, in any combination. All three parts of the mobile spine can be affected, but the lumbar and cervical regions are much more likely to cause symptoms. This is due to the relative mobility and loads placed on these regions.
Symptoms cause pain that usually worsens with loading and lifting and is relieved by rest or flexed positions. Arm or leg pain is very common and, when more severe, there may be limb numbness or weakness or hand dysfunction. The distribution of pain or neurological symptoms is determined by the affected nerve and depends on whether the disc is of cervical, thoracic or lumbar origin. When spinal cord compression is present, gait, balance and continence may be affected. Surgery is recommended when there is a significant neurological problem or if the pain does not respond well to simple measures. Simple discectomy, microdiscectomy, minimally invasive discectomy or anterior cervical discectomy and arthrodesis can be very effective in selected patients who do not respond to rest, analgesia and other conservative measures.
Another problem that commonly affects the disc is degenerative disc disease which can cause disabling symptoms such as pain, loss of limb strength, difficulty walking, etc. This can affect any region or area of the spine, but mainly the cervical and lumbar spine. These problems may require treatments ranging from physical therapy to complex surgeries involving disc replacement and support with screws.
Neuralgia
When a spinal nerve is compressed, it can cause a very characteristic pain. It is often quite severe and it usually depends on the position. The distribution and character of the pain can help determine which nerve is being compressed. Especially for patients who do not respond well to rest and medications, surgical decompression of the affected nerve can be very effective in treating the pain. Up to 90% of carefully selected cases will feel complete or near-complete relief.
Back pain
Even though back pain is very common, it can be caused by a number of conditions and it is thus not always possible to identify the cause with absolute certainty. Intervertebral discs, vertebral bodies and facet joints are common sources of back pain. When conservative treatment fails, surgical intervention may be considered only when the source of the pain can be identified with confidence. Sometimes additional tests (e.g. discography) are required to establish which patients will benefit from intervention.
Facet joint disease
The facet joints are important components of the spine that ensure stability and allow for a safe range of motion. When these joints are affected by the disease, there is usually joint enlargement and fluid buildup, which often results in the narrowing of the spinal canal and compression of the underlying nerves. Synovial cysts may occur under the joint. There may be referred pain from the joint. When there is related isolated pain, facet injections may be an option. Common surgical treatments include cyst resection, facetectomy, laminectomy, or fusion procedure.
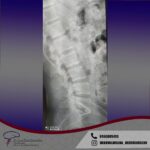
Instability and deformity
Abnormal alignment or angulation of the spine can cause disabling symptoms. The most common form of this is the result of wear and tear changes affecting the intervertebral discs and overlying facet joints. This can result in the movement or displacement of one vertebra relative to its neighbor, a phenomenon known as spondylolisthesis. A congenital form of this is also seen in the lumbar spine and results from a defect in the bridging bone called the pars. When symptomatic or progressive, a decompression or fusion procedure can be very effective. Generally, an instrumented fusion would be recommended in these cases.
Trauma
Spinal injury is a very common cause of back and neck pain. This can range from major trauma to minor whiplash injuries or even sudden changes in position. The result can be bone fractures or crush injuries, facet injuries, and ruptured ligaments or discs. The starting point is to define the injury, the mechanism, and the structures involved as precisely as possible. However, it is not always possible to clearly define the cause of the pain, as is the case with some whiplash injuries. Stable injuries can be treated with rest and immobilization with special collars and braces, followed by serial imaging. Unstable injuries require surgery. Commonly used surgical strategies include anterior cervical discectomy and fusion (ACDF), corpectomy, instrumented fusions, and lateral mass fusions.
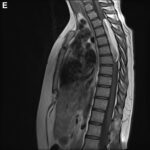
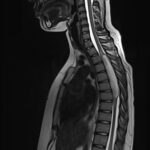
Spinal tumors
Tumors can affect the spinal column or vertebrae, as well as the contents of the spinal canal; the spinal cord, nerve roots, and epidural tissues. The most common symptoms caused by these tumors are cancers in the form of metastatic deposits. These tumors may manifest in pain from nerve compression or fracture or in spinal cord/nerve dysfunction. Primary bone tumors of the spine, such as chordoma, sarcoma, or chondrosarcoma, are much less common. Often, a combination of surgery and radiation is required. Hemangiomas are common benign tumors of the spine. They are sometimes symptomatic and if so, may also be considered for treatment.
Other tumors arise from the spinal cord coverings (or membranes) or from within its substance. Meningioma, schwannoma, neurofibroma, astrocytoma, and ependymoma are the most common types. Surgery is usually required to make a diagnosis, to remove pressure effects from the spinal cord and nerve roots, and sometimes to provide stability. Tumors can be subclassified according to location and structure of origin into intradural, extradural, intrinsic or extrinsic.
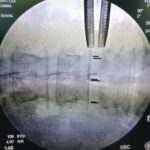
Microdiscectomy / Foraminotomy
When compressed, spinal nerves become symptomatic and start producing pain. Often, a prolapsed disc will push the nerve against an overlying bony structure. A microdiscectomy is the procedure in which the small problematic portion of the prolapsed disc is removed using magnification and a unilateral (one-sided) approach. The foramen refers to the tunnel through which the spinal nerves leave the spinal canal. When the nerve is compressed here, part of the tunnel is opened to relieve the nerve. This is called a “foraminotomy”.
Laminectomy/ Hemilaminectomy
The laminae form part of the posterior annulus structure of each vertebra that surrounds the spinal cord and central neural structures. A laminectomy removes part of this annulus to allow access to the compressed structures below. When canal stenosis is present, this alone is usually sufficient to treat the symptoms. When symptoms are one-sided, surgery can be further minimized by removing only a portion of this posterior ring, the “hemi-lamina”. Indirect access to the contralateral (opposite) side can also be achieved.
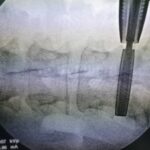
Minimally invasive surgery
This term refers to a new way of performing spine surgery, with the aid of tubular retractor systems instead of through an open incision. It is designed to minimize muscle trauma and shorten postoperative recovery times. In my opinion, the trade-off may be exposure and safety. The technique should be used selectively. In this regard, we offer our patients practically the entire current world-class gamma of minimally invasive techniques to resolve spinal pathologies. The minimally invasive techniques we offer range from herniated disc surgery to complex instrumentation to replace discs or vertebral bodies by different routes of minimal access (anterior abdominal, lateral abdominal, posterior) and placement of percutaneous support screws (entering through minimal holes in the skin).
Motion preservation spine surgery
Each segment of the spine allows small motions through the intervertebral disc and facet joints. This allows flexion and extension as well as lateral bending and some rotation. These movements, when combined in many segments, allow us to perform all our usual daily activities. Whenever possible, simple procedures are preferred over fusion operations to preserve this motion. However, if the main problem is with the disc or abnormal motion, then a fusion may be the most appropriate intervention.
Instrumented fusion
A fusion is designed to permanently connect two or more segments. This procedure is recommended when the interposed disc is the source of the back pain or if there is obvious instability or movement along the level. The most common way to do this is with titanium pedicle screws, fixed with rods and sockets. At the time of surgery, bone grafts and supplements will be placed to allow for bony fusion. Over time, this will provide the strength of the fusion. Alignment and curvatures can also be corrected with instrumented fusions.
Extraforaminal and lateral discs
Occasionally, a prolapsed disc will be outside the normal spinal canal and will affect the course of the nerve at this location. The nerve is very sensitive at this point in its course and for patients with severe or refractory symptoms, surgery can be very effective. A special approach is used to correct the problem.
Services in Quito
Spinal cord and nerve surgery
Correction of spinal cord and nerve anomalies that require surgical intervention
Diseases of the spinal cord that require surgical treatment
In the sections on spinal pathologies, we can see that certain patients may have implicit damage associated with the spinal cord caused by the trauma of the spinal column for instance. In many patients, a corrective surgery that was done on time can make the difference between a functional recovery or not of the spinal cord. Here, I will mention the pathologies that originate from the spinal cord itself or that affect it by contiguity; pathologies that I am very passionate about solving. Basically, the main diseases I will discuss are spinal tumors and syringomyelia.
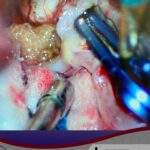
Spinal cord tumors
These tumors can be divided into intradural and extradural tumors. Intradural tumors are found inside the compartment where the spinal cord is located, that is, inside the outermost envelope called ‘dura mater’. These in turn are divided into intramedullary (originating from the spinal cord tissue itself) and extramedullary tumors. This last group is found in the same compartment of the spinal cord and can usually compress it and compromise its function, but they do not originate from it. The two most common intramedullary tumors are ependymomas and astrocytomas. The most representative intradural extramedullary tumors are meningioma and neurinoma. There are also other, less common lesions in both groups that can be resolved with considerable solvency when we see them in our daily practice.
Ependymomas and astrocytomas are lesions that usually require surgical intervention, but depending on their histopathological characteristics that define whether or not they are benign, they may require supplementary treatment based on chemotherapy or radiotherapy to achieve better cure and/or survival rates. These lesions should be resected, in addition to microsurgical vision with neurophysiological surveillance that improves the results.
I suggest you consult the ‘cases’ section below, where you can find an example of an operation of a very particular and rare intramedullary tumor that yielded excellent results.
Meningiomas and astrocytomas are usually benign lesions, but due to their growth and compression of the spinal cord, they can have devastating functional consequences, such as impeding the movement of the limbs and thereby partially or totally disabling the patients. Fortunately, adequate resection (exeresis) can solve the problem and we have ample experience in these pathologies.
Extradural tumors affect the bony tissue of the vertebrae as well as the adjacent soft tissues (ligaments, muscles, etc.). However, substantial growth could also affect the spinal canal and nerve structures. This group of extradural tumors includes bone tumors (primary vertebral) and metastases. The first group consists of both benign and malignant lesions that require actions ranging from biopsy, resection alone or supplemented with chemotherapy and/or radiotherapy.
Metastases are lesions that imply the presence of another distant or systemic tumor. They affect or invade the spine and may have a malignant context. Their treatment depends on the vertebral and neurological involvement of the patient; they may require from a simple biopsy to decompression of neurological structures, partial or total resection that may even require instrumentation (prosthesis placement) to maintain the alignment and balance of the spine.
Syringomyelia
It is a disease of the spinal cord that consists of an abnormal dilatation inside the spinal cord with excessive accumulation of fluid that affects the sensory and motor functions causing a great variety of symptoms and disabilities in patients. Several theories explain the cause as an alteration in the cerebrospinal fluid circulation, which can be the result of various lesions such as spinal tumors, congenital malformations, trauma or even idiopathic (unknown). It is often necessary to treat the underlying pathology or to perform surgery directly on the syringomyelia by relieving the internal pressure in the spinal cord – usually by draining and shunting the excess fluid out of the abnormal space. These treatments can provide significant relief and improvement, which in turn can restore patients’ functionality. They can also prevent neurological deterioration when it has already begun.
Carpal tunnel syndrome (CTS)
The median nerve passes through a tunnel as it enters the hand. If the boundaries of the tunnel become filled, the contents become compressed and the function can be impaired. The median nerve is the most sensitive of these structures and, when compressed, there may be neurological and pain symptoms affecting the hand and forearm. Diagnosis is made clinically and with the use of electrodiagnostic. Surgery is simple and necessary in all cases but very mild ones. In this type of surgery, known as carpal tunnel decompression, the superficial roof of the tunnel is opened and space is created for the underlying nerve. I suggest you consult the ‘cases’ section below for an example.
Ulnar neuropathy
The ulnar nerve is often compressed in a ligamentous (fibrous) tunnel that runs around the inside of the elbow. Symptoms and signs are characteristic and the diagnosis is confirmed with nerve conduction tests. Surgery consists of an ulnar nerve decompression, that is, opening the tunnel and, in some cases, moving the nerve to a safer nearby location.
Trigeminal neuralgia
When the trigeminal nerve (nerve for facial sensation) is compressed by a nearby artery, a pain syndrome called “trigeminal neuralgia” can develop. This results in episodes of excruciating pain affecting one side of the face. When symptoms are poorly controlled with medication, then a relatively simple operation, in which the affected artery is separated from the trigeminal nerve with a small piece of inert material, is very effective in relieving the pain. This operation is called microvascular decompression. I suggest watching a video of this case below in the ‘cases’ section.
Hemifacial spasm
Hemifacial spasm is an uncommon case of irritation affecting the large motor nerve called the facial nerve. It results in involuntary movements of various parts of the face, usually starting with the eye muscles. Some medications can be effective and many patients benefit from percutaneous Botox injections in the short term. When these measures fail, surgery can be very effective in providing a permanent solution. Usually, a nearby arterial loop is found that compresses the nerve near its origin. The loop is gently removed from the nerve and a soft dressing is placed to keep it away. The long-term results are very good. Nevertheless, the procedure entails a small risk of hearing loss on the same side. I suggest watching a video of a case example in the ‘cases’ section below.

03. Spinal cord and nerve surgery
Cases In Quito
Demostrative cases
01. Brain surgery
02. Spine surgery
Address
Hospital de los Valles: Cumbayá
Appointments
096 841 4286
doctor@duvalmolina.com